Authors
Theresa Schmidt, MA; Tom Valuck, MD, JD; Jacqlyn Riposo, MBA; Palak Patel, MHA; Brittany Perkins, MPH; Kimberly Westrich, MA; Robert W Dubois, MD, PhD.
Publication
Journal of Clinical Pathways, 2022;8(8):33-43. doi:10.25270/jcp.2022.12.01
December 2022
Shared decision-making (SDM) and patient decision aids (PtDAs) may reduce costs or improve utilization but not consistently across settings and diseases, according to a new systemic literature review by researchers from National Pharmaceutical Council (NPC) and Real Chemistry.
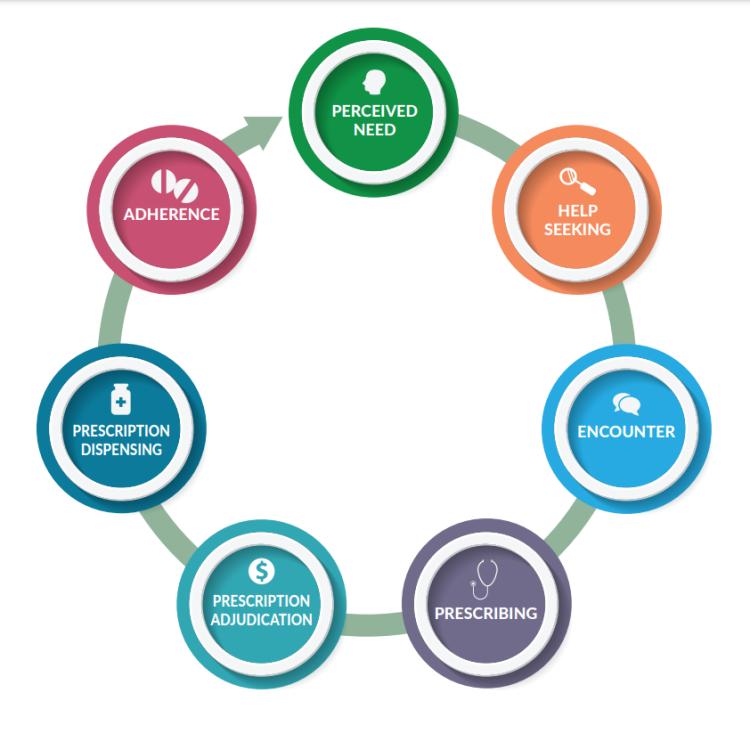
Prior research supports the use of shared decision-making (SDM) and patient decision aids (PtDAs) to promote patient-centered, high-quality care. However, the impact on costs and utilization, and furthering the goals of value-based care embedded within the Affordable Care Act, is less clear.
To examine this issue, researchers from NPC and Real Chemistry conducted a systematic literature review examining the available evidence regarding evidence on the impact of SDM as a process, PtDA as tools to support decision-making, and the combination of SDM and PtDAs on cost, utilization, and prevention-related care.
The 51 articles reported outcomes of interest as follows across the three main categories: cost (N=8), utilization (N=25), and prevention-related care (N=32). Thirty-nine articles had outcomes in only one category, 10 had outcomes in two categories, and only 2 articles had outcomes in three categories. A single article can have outcomes in multiple categories.
- Cost: Of the outcomes evaluated pertaining to a dollar amount, 5 show a cost decrease, and 6 show no difference.
- Utilization: Of the outcomes addressing impact on resource-intensive services or procedures, 14 show a decline, and 9 show an increase in use of services or procedures.
- Prevention-related Care: Of the studies that address outcomes involving processes or procedures that could potentially improve other health outcomes and reduce future high-cost utilization, 20 reported an increase in prevention-related care and 21 reported no difference.
Of the three outcomes, the use of prevention-related care increased the most due to SDM and PtDAs, compared to cost and utilization outcomes.
This review indicates variation in evidence of the impact of SDM and PtDA on healthcare costs and utilization, but the majority of findings indicate costs and overall utilization were reduced or static, and prevention-related care increased or was unaffected. Prior research has shown the relevance of SDM and PtDAs for promoting better care and healthy people/healthy communities. Our systematic review found that these interventions may also be positioned to support the health system’s shift to value-based care models.