What’s the challenge with utilization management and step therapy strategies?
We know that every patient is unique. The challenge with utilization management strategies is that the decisions health care providers make for individual patients can collide with “one size fits most” approaches designed for the “average patient.”
In particular, step therapy – often referred to as “try and fail” – can lead to delays in care. Those delays in accessing a treatment that works might hold minor consequences for someone with seasonal allergies. However, the consequences might be significant for a patient with rheumatoid arthritis, for example.
Those health impacts may translate into higher costs over time. Though health plans might see short-term drug cost savings using step therapy, those gains may be lost to long-term increases in hospitalizations or treating worsening conditions.
Step therapy can be burdensome for both patients and health care professionals, taking time away from patient care or leading patients to abandon treatments that could yield better health outcomes.
Variable approaches lead to inconsistent access.
A study published in Health Affairs and conducted by NPC and the Center for the Evaluation of Value and Risk in Health at Tufts Medical Center examined the utilization management strategies used by commercial health plans in the U.S. Study authors found only 15.9% of drug coverage policies were consistent across the largest U.S. commercial health plans. Less than half (48%) of all drug coverage decisions were consistent across 75% of health plans.
These variations in how health plans manage access to specialty medications can impact patients and mean that treatment might be significantly disrupted for patients whose conditions are controlled on one treatment but the patient switches health plans or employers.
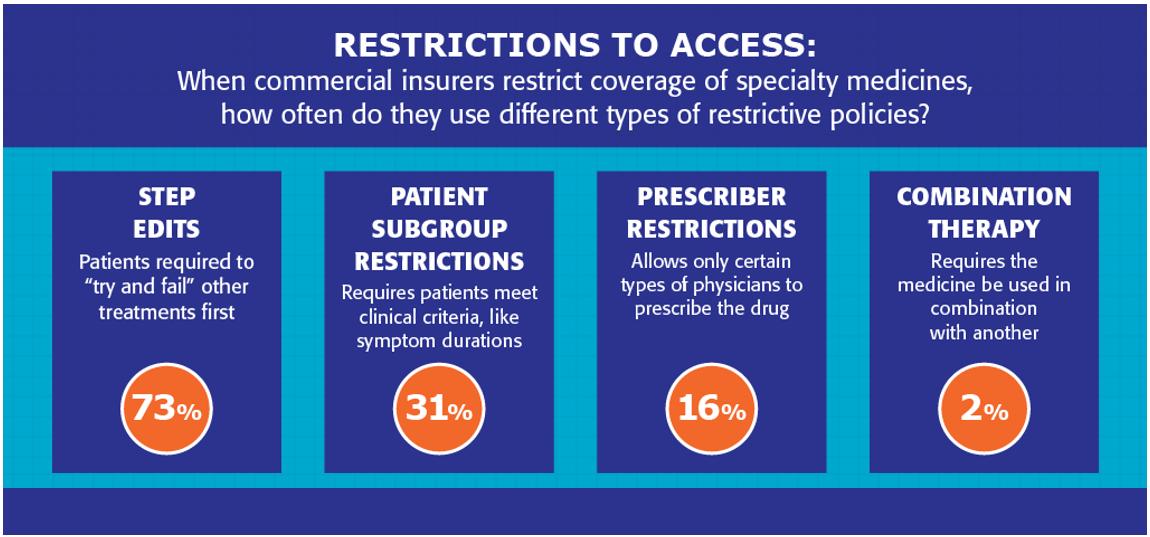
The study also highlighted the restrictions to access patients most often face. “Step edits,” policies that require a patient to try one or more other medications first and fail on those treatments, were the most common access restriction imposed. On average, patients with plans incorporating step edits were required to try and fail 1.5 prior therapies before coverage of the specific medication indication was allowed.
The Need for Common Standards
The COVID-19 pandemic put a clear spotlight on the risks of putting up excessive barriers to necessary care for patients. The opportunity for health plan decision-makers is to consider how to implement step therapy in a way that successfully promotes clinically recommended and safe care while also ensuring affordable access.
A study led by NPC explored that question in a paper published in the Journal of Managed Care & Specialty Pharmacy. Currently, there are no common standards for developing step therapy protocols. The NPC research team convened a group of 16 stakeholders and experts—representing the patient, physician, payer, pharmacy, health policy and ethics communities—to determine what should define appropriate step therapy standards and to see whether a diverse group of stakeholders could agree on what these standards should include. The recommendations – focusing on areas like evidence, implementation and transparency – can serve to help health plan decision-makers employ balanced approaches.
