What are value-based contracts?
Value-based contracts are one of many alternative payment mechanisms that can help achieve cost savings and improve patient outcomes in the United States. They can promote greater patient access to new biopharmaceutical treatments by linking reimbursement, coverage, or payment to a treatment’s real-world performance. For value-based payment models to achieve their full potential, regulatory barriers (e.g., Medicaid Best Price), as well as challenges related to the implementation of these contracts must be addressed.
Value-based contracts rely on an innovative new payment model that brings together two key stakeholders—health care payers and biopharmaceutical manufacturers— to deliver medicines to patients. Through value-based contracts, biopharmaceutical manufacturers and payers agree to link coverage and reimbursement levels to a medicine’s effectiveness.
Value-based contracts are sometimes referred to as risk-sharing agreements, value-based arrangements, or outcomes-based contracts.
What are the benefits to stakeholders?
Payers, manufacturers and patients all have different interests in the development and use of value-based contracts.
Benefits to payers:
-
Value-based contracts allow payers to gain experience with a product, reducing uncertainty regarding clinical value, performance, and financial impact.
-
By basing payment on a product’s real-world performance, value-based contracts can reduce a payer’s risk of making a sub-optimal purchase.
Benefits to manufacturers:
-
Manufacturers can use value-based contracts to differentiate and demonstrate the effectiveness of their product, particularly within a crowded therapy class.
Benefits to patients:
-
Value-based contracts can help provide earlier access to biopharmaceuticals for patients and consumers, particularly for treatments that serve small patient populations and have limited clinical data.
-
Value-based contracts can also improve patient access to new medications and treatments by providing an alternative to closed formularies.
How are value-based contracts being used?
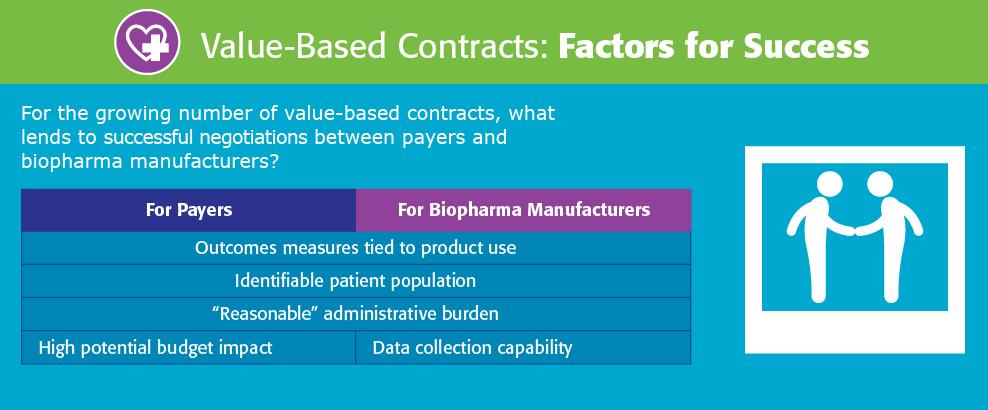
In the United States, value-based contracting activity in the public domain has been relatively limited. But interest in these agreements among both payers and biopharmaceutical manufacturers is strong, and a changing health care environment may generate more activity in this arena in the future. The National Pharmaceutical Council partnered with the Duke-Margolis Center for Health Policy to survey payers and biopharmaceutical manufacturers on their participation in value-based contracts. The study, published in 2019, found that most value-based contracts are not publicly disclosed, indicating that the implementation of this model is more prevalent than previously assumed.
What are barriers to broader implementation?
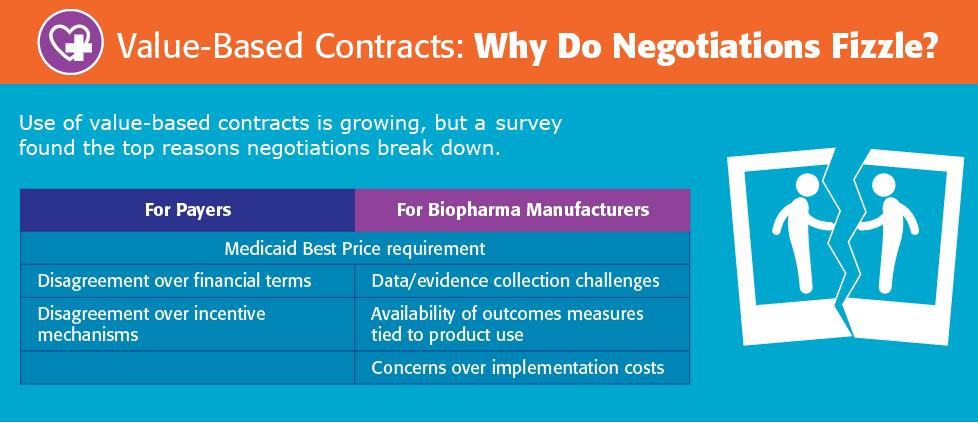
Despite growing stakeholder interest in value-based contracts, regulatory barriers and challenges in the negotiation process make it difficult to design and implement these contracts in the current environment.
Policy barriers
Unintended consequences of other health care policies like the Anti-kickback Statute and Medicaid Best Price have caused some payers and biopharmaceutical manufacturers to think carefully before entering into value-based arrangements. An NPC analysis published in 2018 conducted quantitative and qualitative assessments of four main regulatory and legal barriers that are standing in the way of advancing value-based contracts in health care and quantified the impact of removing them. Despite some recent regulatory changes, additional reforms are needed for this payment model to be able to achieve its full potential to reduce health care spending.
Challenges with the contract negotiation process
There are also many challenges related to negotiating the terms of value-based contracts, including:
- data collection and evidence development;
- the availability of appropriate outcome measures;
- implementation costs; and
- disagreement over incentive mechanisms and/or financial terms
Potential for the Future
It is likely that there will be more value-based contracting activity in the future. This expansion could be fueled by (1) improved data systems, which can help create the mechanisms to monitor patient usage of biopharmaceuticals and their effect on health outcomes; and (2) changing incentives within the health care system toward value-based orientations. The increased use of accountable care organizations, for example, may lead to enhanced health system alignment with value-based contracts.