Ciarametaro M, Houghton K, Wamble D, Dubois RW.
Value in Health, March 3, 2021
This study assessed the potential effects of budget caps design on disease burden and cost savings in order to help budget decision makers understand which budget cap features minimize impact to patient health. A budget cap is a tool designed to help policymakers plan the next year’s budget and set limits on annual health spending growth in relation to annually projected health care costs.
Currently, there is no clear understanding of which budget cap factors are the most import for success, and no uniform way of how budget caps get implemented. This study helps to identify which features are needed to ensure success, both in terms of cost reduction and health improvement. States are increasingly using health care budget caps to limit spending and manage spending growth, and this study can help inform budget decisions made by state Medicaid directors and state legislators.
Methods:
To assess effects, researchers applied different budget cap types (global vs. service level) and annual cap growth strategies (general vs. disease specific) to eight of the commonly occurring medical conditions in the United States from 2005-2015. The conditions selected for the study were ischemic heart disease, breast cancer, cerebrovascular disease, chronic obstructive pulmonary disease (COPD), asthma, atrial fibrillation, and rheumatoid arthritis. The researchers also investigated how differences in condition-specific prevalence and outcome trends affected the impact of budget caps on patient health.
Three different hypothetical annual budget cap growth strategies were applied across all eight conditions at both the aggregate health care spending level (total cost of medical care) and the aggregate drug spending level (only the cost of prescribed medicine). The first approach limited annual growth to the Consumer Price Index for All Urban Consumers (CPI-U), the second approach used CPI-U plus a yearly adjustment for overall US population growth, and the third used CPI-U plus a yearly adjustment for condition-specific–estimated prevalence. Both health impact and cost savings were examined for each of the three scenarios.
Health was assessed by a measure of disease burden – disability adjusted life-years (DALYs). The DALY allows for comparisons of the burden of illness experienced across different diseases. One DALY is the equivalent of one year of healthy life lost if a person had not experienced the disease.
The researchers identified the smallest and largest DALY differentials in order to determine both the minimum and maximum health impact that the budget caps may produce. The higher the DALY score, the greater the disease burden for the year of interest (the DALY does not project future disease burden).
Results:
The results indicate that budget caps have the potential for creating savings but can also result in patient harm if not designed well. Pharmaceutical level budget caps, when compared to aggregate budget caps, lead to worse health outcomes in all cases.
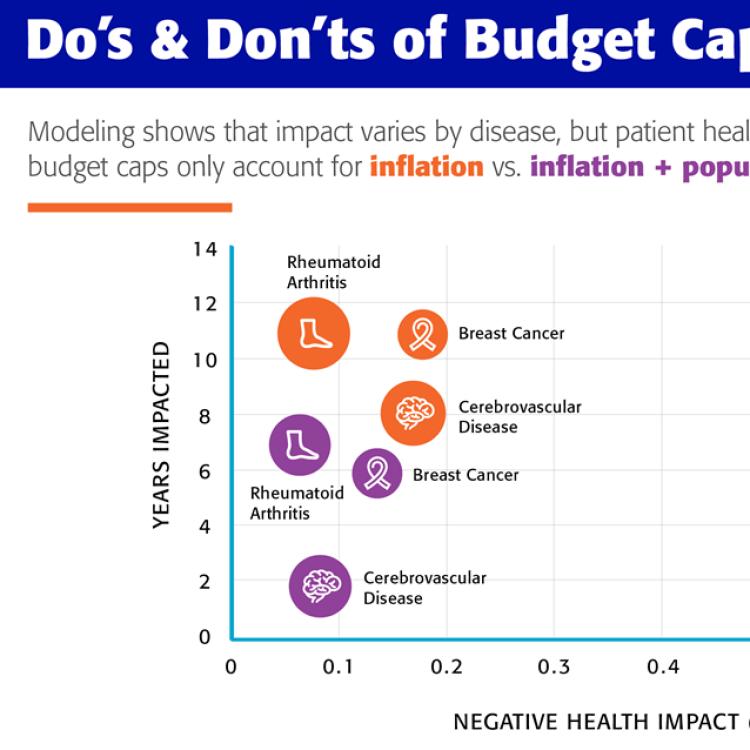
The first hypothetical budget cap growth strategy, which included an inflation adjustment using only the CPI-U, had the greatest potential for negatively impacting patient outcomes. Applying this approach for aggregate-level expenditures at the disease level led to smaller per-person budget projections which resulted in patient harm for some of the conditions. The negative effects intensified when imposed at the pharmaceutical or medication spending level. This shows that CPI-U only annual budget growth targets are not adequate, and annual changes in health spending are better predicted by a combination of inflation and changes in population or disease prevalence.
The second and third hypothetical budget cap growth strategies performed better, with fewer projected consequences to patient outcomes than the first method. However, once again, the aggregate-level budget caps had less impact (reduced health) than the budget cap that was posed at the pharmaceutical level.
The conditions impacted under the budget cap scenarios shared several disease-specific characteristics. First, conditions that have experienced significant growth in prevalence, such as breast cancer and rheumatoid arthritis, demonstrated significant potential for harm as a result of imposed budget caps. Second, potential patient harm was seen in conditions experiencing a drop in DALYs per person over time (improved health) such as breast cancer, rheumatoid arthritis, and cerebrovascular disease.
Conclusion:
As a result of these findings, researchers developed the following principles that can help guide the design of budget caps in a manner that avoids negative health consequences and addresses medical spending:
- Budget caps should be applied at the aggregate health spend level and not at the individual service level such as pharmaceutical spending. Pharmaceutical level caps could result in worse patient outcomes, particularly for conditions like ischemic heart disease, where actual drug spending has increased yet overall spending for the condition has declined because of better drugs.
- Budget caps should be adjusted to consider both inflation and changes in population or prevalence specific to the condition or disease state. Budget caps that only account for changes in inflation year over year, such as CPI-U, should be avoided. CPI-U–only approach to setting a spending target will result in the greatest potential for negatively impacting patient outcomes.
- When considering budget caps, changes in per-person health, spending and disease prevalence should be analyzed regularly to determine which conditions have the greatest potential for harm as the result of budget targets. It is critical to institute appropriate protections such as excluding select conditions from budget caps when health is improving, and the budget is growing.
- Properly designed budget caps can be considered in conditions where costs are growing, and health is not improving. Active monitoring of new medical technologies should be incorporated so that funds can be available for new medical technologies that are high value.
- Budget caps do not uniformly impact diseases. No matter the design, budget caps create the potential to harm patient health in some conditions.
- It is important to incorporate appropriate quality metrics to actively monitor patient health. The focus of quality metrics should be vulnerable populations such as those with diseases undergoing prevalence increases or significant changes in patient health over time.
- Considerable variability at the condition level, including patient population, treatment costs, and the innovations available, means that budget caps have the potential to both create savings and harm. Short-term cost benefit should not come at the detriment of population health in the long term.
Limitations:
The authors of the study pointed out several limitations, including:
- The study does not allow for public health care policies that effect the prevalence and outcome of conditions, nor interventions that may reduce overall burden.
- The DALY was developed as a way of comparing the overall health and life expectancy of different countries and conditions. It was not developed as a measure for individual patients, and it does not incorporate specific disease-related factors in its calculation.
- The study’s budget cap approach did not account for any changes in health care provider behavior that may directly impact health outcomes and resource use.
- The study assumed a one-to-one relationship between budget cap impacts on spending growth and patient health gains (e.g. a 15% decrease in spending growth would lead to a 15% decrease in any health gains).
- Total cost of care and biopharmaceutical spending caps were modeled.