With health care spending in the United States approaching 20% of GDP, a lot of efforts are underway to keep this spending under control. One of the less talked about strategies that’s gaining traction in the U.S. at the state level is the use of budget caps – a budget planning tool designed to help policymakers set a limit on annual health spending growth in relation to annually projected health care costs.
Researchers from the National Pharmaceutical Council (NPC) and the Research Triangle Institute Health Solutions (RTI-HS) conducted a study to show how budget caps may impact patients’ health. Their research paper, “The Dollar or Disease Burden: Caps on Healthcare Spending May Save Money, but at What “Cost” to Patients?”, was published in the latest issue of Value in Health.
The study provides guidance on quality metrics and practices that can help budget decision makers, state medical directors and state legislatures understand which budget cap features have the potential to lessen the impact on patient health and provides recommendations that could reduce any damage.
Several states – New York, Pennsylvania, Maryland, Delaware, Massachusetts, Rhode Island, Vermont and California – are increasingly using budget caps to contain health costs and manage health budgets more efficiently.
However, depending on the approach policymakers use, budget caps may have the potential to do more patient harm than good. The central goal of budget caps is to limit spending growth, which could lead to a negative effect on the growth of innovation.
“Innovation is a key driver of improved patient health and roughly one-third to slightly less than two-thirds of annual spending growth supports innovation,” said Michael Ciarametaro, a co-author of the study and Vice President of Research at NPC. “Budget caps aim to reduce annual spending growth, and, as a result, may stifle innovation and harm patient health if important factors such as underlying trends in patient health are not considered.”
In addition, the way the caps are implemented and enforced, and how the spending growth is measured, varies state by state. States often set budget caps growth targets using non-health factors such as inflation, productivity growth and GDP growth.
The researchers explored the health impacts of budget caps across three annual growth strategies over a 10-year time frame for eight of the most commonly occurring conditions in the U.S. – ischemic heart disease, breast cancer, cerebrovascular disease, chronic obstructive pulmonary disease (COPD), asthma, atrial fibrillation, and rheumatoid arthritis.
Impact on health was assessed by a measure of disease burden DALYs (disability adjusted life-years), a numerical value between zero and one that represents one year of perfect health lost. A value of “zero” means there is no impact on patient health, while “one” means a patient lost one year of perfect health.
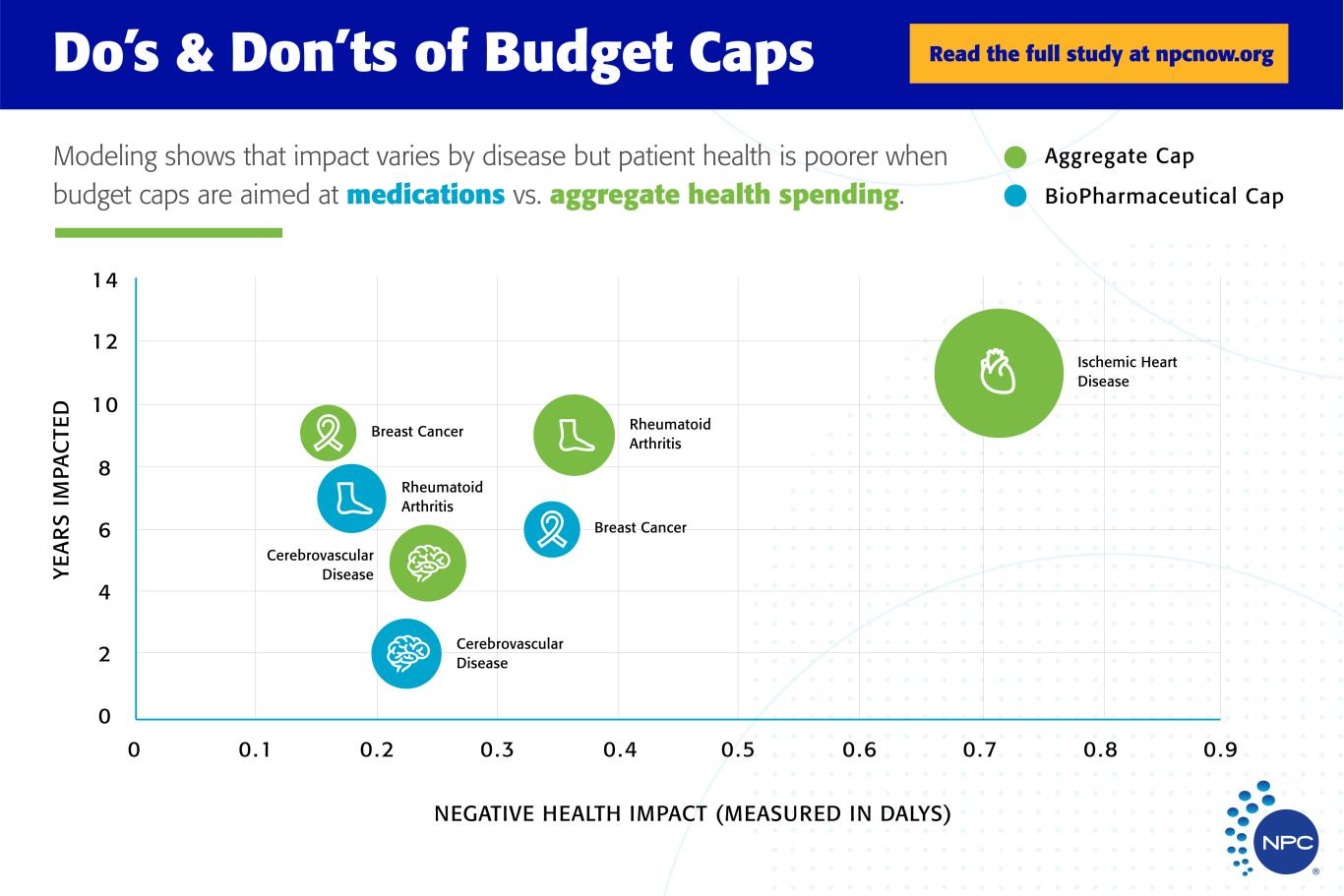
The researchers looked at two budget cap models – one that sets limits based on total cost of care for all health services, and a second that limits only biopharmaceutical prescription drugs costs. They wanted to understand how these two types of caps perform, and how a budget cap allows spending to grow year on year. They modeled spending based on annual inflation rates, population growth and prevalence of specific disease areas.
The findings showed ways how budget caps could affect patient health and what can be done to avoid further harm:
- Biopharmaceutical budget caps created more patient harm than total cost of care budget caps – budget caps should not be applied at the pharmaceutical spend level.
- The inflation rate-only approach to setting a spending target will result in the greatest potential for negatively impacting patient outcomes – budget caps annual growth rates should be adjusted for both inflation and population growth or disease prevalence changes.
- Budget caps do not uniformly impact diseases – no matter the design, budget caps have the potential to harm patient health in some conditions.
- Quality metrics like those used in the Centers for Medicare and Medicaid Services (CMS) Oncology Care Model are needed under the following conditions:
- diseases where patient health at a population level is improving year on year.
- diseases where there are meaningful increases in prevalence.
- Conditions impacted under the budget cap scenarios shared several disease-specific characteristics:
- conditions that experienced significant growth in prevalence, such as breast cancer and rheumatoid arthritis, demonstrated significant potential for harm because of imposed budget caps.
- a drop in DALYs per person over time was seen in breast cancer, rheumatoid arthritis, and cerebrovascular diseases.
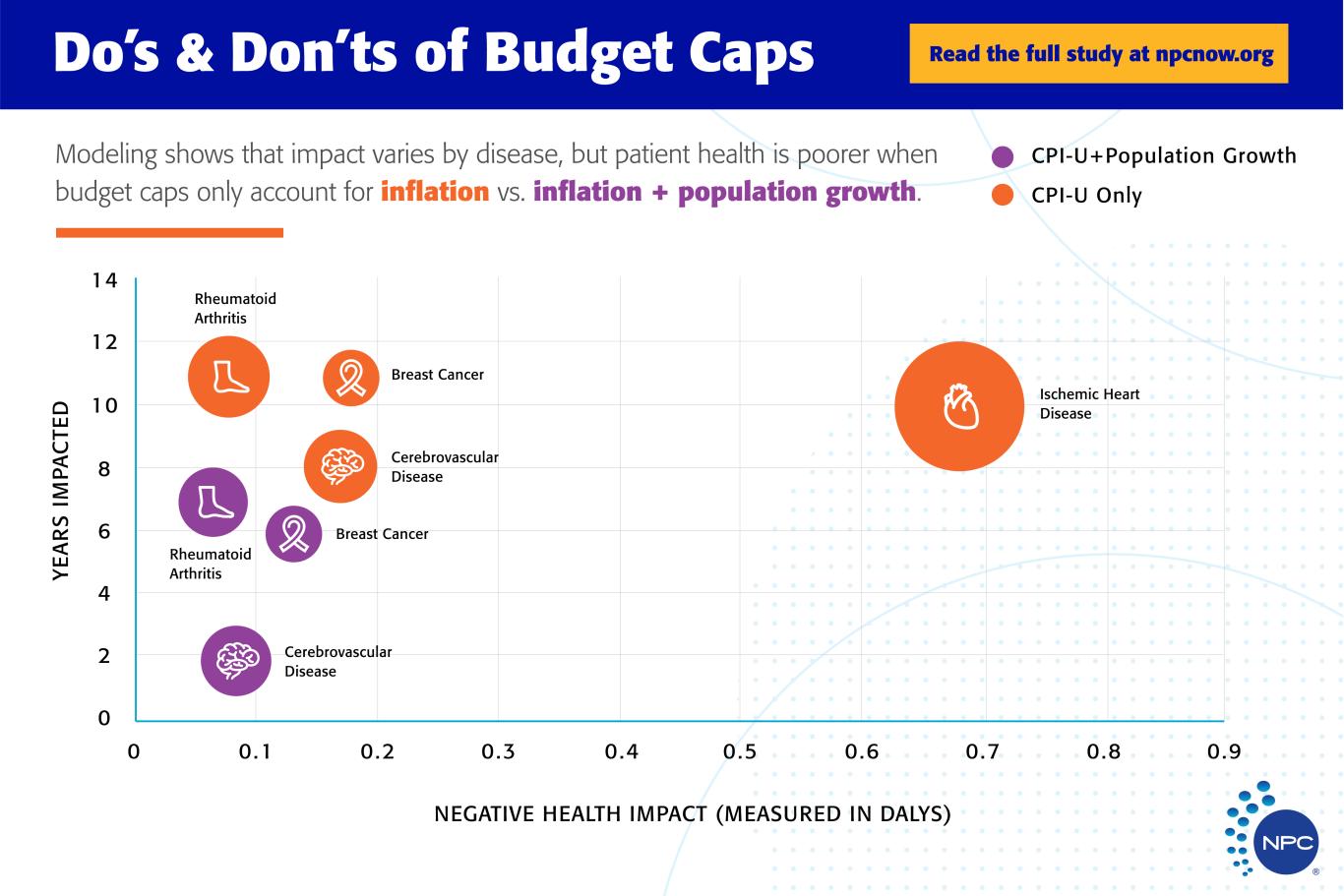
“What surprised me the most is the potential harm that can happen to patients when budget caps are only adjusted by inflation,” said Mr. Ciarametaro. “This study provides some clear practices that may be used to reduce the harm to patients from budget caps. States will be helped the most by the study since that’s where the majority of budget caps use exists.”
If not done in a more thoughtful way, budget caps could worsen health outcomes by not encouraging innovation that could improve patients’ health. Caps also could harm patients if they’re not designed well. The researchers hope that the principles they developed from this study can guide the use of budget caps to improve patient health and avoid the negative consequences that can result from this approach to controlling health care spending.